- The added value of clinical laboratories in personalized medicine: the evidence
- New IFCC App is now available for download
- The IFCC e-Academy
- Shaping the Future of Laboratory Medicine
- IFCC Foundation for Emerging Nations
- C-AQ – C-CLM: What is the best strategy to achieve compliance with QMS- and QC-requirements in the clinical laboratory?
- ICE Award
- Visiting Lecturer Programmes in Cuba, Zimbabwe and Romania
- Task Force Young Scientists Session on “Scientific Writing” at Medlab 2016, Harare, Zimbabwe
- NEWS FROM REGIONAL FEDERATIONS AND MEMBER SOCIETIES
- Pakistan Society: CME Seminar on World Rare Disease Day
- XX Congress of Medical Biochemistry and Laboratory Medicine and 12th EFLM Symposium for Balkan Region
- The STBC celebrates its 35th birthday in Hammamet!
- News from SEQC: EQALM symposium 2016
- Finnish Society of Clinical Chemistry celebrates its 70 anniversary
- New Uruguayan Association of Biochemistry Executive Board
- EFLM at the 14th APFCB Congress in Taipei
- EFLM-BD Walter Guder Award and CCLM Award
- EFLM Task and Finish Group on CPD Crediting System
- An update on the activity of the EFLM Working Group on the Preanalytical Phase
- Calendar of the next EFLM webinars
- EFLM bursary programme
- IFCC Travel Scholarships at IFCC General Conference in Madrid
- IFCC Calendar of Congresses, Conferences and Events
IFCC eNews July – August 2016
Listado de emisiones anteriores
Screen all adults for Hepatitis C, say researchers
Based on their findings among nearly 5,000 patients seen at the Johns Hopkins Hospital emergency department, researchers are recommending universal hepatitis C virus (HCV) screening for all adults ages 18 and older. If implemented, this recommendation would identify up to 25% of individuals with undiagnosed HCV infection who would not be detected by current screening guidelines, according to the investigators. Their findings were published in the journal Clinical Infectious Diseases.
Many people with hepatitis C have no noticeable symptoms and don’t know that they are infected. Left untreated, HCV infection can progress and cause chronic liver damage. Screening can help identify those who are unaware that they have hepatitis C so that they can receive treatment.
Currently, the Centers for Disease Control and Prevention (CDC) recommends one-time testing for all individuals born between 1945 and 1965, the so-called baby boomers. This is in addition to the agency’s long-standing screening recommendations for people at high risk of hepatitis C infection. These include individuals with HIV as well as those with a history of injection drug use, dialysis, blood transfusion, or transplants. Children born to women with hepatitis C and individuals with persistently abnormal liver enzyme (alanine aminotransferase, ALT) levels should also be tested for HCV.
Screening involves testing a person’s blood for antibodies produced in response to HCV infection. This antibody test can be positive whether a person has an active infection or has been exposed to the virus in the past. A second, different test that directly detects HCV RNA must be done to confirm the presence of the virus and diagnose an active infection. About 70% to 85% of people who are positive for the antibody will also have a positive HCV RNA test.
Research studies conducted prior to the Johns Hopkins investigation have reported high numbers of people with positive HCV antibody tests, from 13% to about 18%, in urban emergency department populations. The researchers wanted to determine the overall impact of HCV infection and evaluate how effective the CDC recommendations are in detecting people with unknown HCV infections in their urban emergency department.
The 8-week study involved screening for HCV in all patients at least 18 years old who visited the emergency department. Of 4,713 unique patients with blood samples taken as part of routine care, 13.8% were positive for hepatitis C antibody, indicating exposure to the virus. Nearly one-third of these individuals had undiagnosed HCV infection.
Of those with undiagnosed HCV infection, nearly half would have been diagnosed based on current CDC age-based testing, while 26.5% would have been identified based on risk factors, including injection drug use and HIV infection. However, just testing in accordance with CDC guidelines would have missed 25% of cases.
Among those who would have been missed by current screening recommendations, the researchers found an increase in the number of non-black men and women born between 1979 and 1995—much younger than the baby boomer group—who tested positive for HCV antibody (7.6% and 5.7%, respectively).
The researchers calculated that at Hopkins, the 13.8% overall positive hepatitis C antibody rate would equate over the course of a year to about 8,000 unique HCV antibody-positive patients and 6,700 with chronic HCV infection.
Without detection and treatment, chronic hepatitis C can lead to other serious conditions. About 60-70% of people with untreated hepatitis C develop chronic liver disease and roughly 20-40% will develop cirrhosis over many years, according to the CDC. About 1-5% of people with untreated HCV are estimated to die from a condition that results from chronic infection, such as cirrhosis or liver cancer.
Hepatitis C can be successfully treated, usually with a combination of drugs. A number of combinations have been approved by the FDA recently, and more are likely to come in the future.
The researchers acknowledged that their proposal to broadly expand HCV testing would demand significant resources but emphasized the importance of identifying patients early in the course of HCV infection. “This is an infection that can now be cured if detected early, rendering people noninfectious and thereby preventing the dire consequences that are associated with the virus,” said senior author Thomas Quinn, MD, a professor of medicine at Johns Hopkins.
Because this study was done in an emergency room setting (where the frequency of infections like HIV, which has similar risk factors, is known to be high) in a city known for having a high frequency of hepatitis C, further studies in other settings would need to be done before deciding whether it would be beneficial to recommend universal screening for hepatitis C.
Source: LabTestsOnline
Obituary: In Memory of Dr Ulisses Tuma, EB Member 2009 – 2014 †
IFCC and the Latin American Community is deeply saddened by the sudden death of Dr. Ulisses Tuma, from Brazil. He passed away on Tuesday, August 23, 2016.
The IFCC has lost one specialist in lab medicine who contributed to IFCC growth in Latin America.
Ulisess Tuma was a Member of IFCC Executive Board from 2012 to 2014. He was a Past-President and Past-Secretary of the Brazilian Society of Clinical Analyses (SBAC) and had served as Chair of the Committee of a number of Brazilian Congresses of Clinical Analyses. He has been very active in a number of other professional organizations serving as a member of the Brazilian Council of Pharmacists-Biochemists and as a member of the executive board of the Association of Superior School of War-State of Goiás-Brazil. Dr. Tuma has also served as the President of Regional SBAC for the state of Goiás-Brazil.
Academically, Dr. Tuma graduated with a degree in Pharmacy-Biochemistry – Federal University of State of Goiás-Brazil. His titles include Specialist in Clinical Analyses by Brazilian Society for Clinical Analyses (SBAC). He has received post graduate training in Cytologyn from the Federal University of State of Goiás-Brazil and in Politics and Strategies from the University of the State state of Goiás-Brazil.
IFCC sincere condolences go to his family and to the Brazilian Society of Clinical Analysis and whole community of Laboratory Medicine specialists in Latin America.
Source: IFCC
Mosquito-borne diseases
Mosquitoes are one of the deadliest animals in the world. Their ability to carry and spread disease to humans causes millions of deaths every year. In 2015 malaria alone caused 438 000 deaths. The worldwide incidence of dengue has risen 30-fold in the past 30 years, and more countries are reporting their first outbreaks of the disease. Zika, dengue, chikungunya, and yellow fever are all transmitted to humans by the Aedes aegypti mosquito. More than half of the world’s population live in areas where this mosquito species is present. Sustained mosquito control efforts are important to prevent outbreaks from these diseases. There are several different types of mosquitoes and some have the ability to carry many different diseases. Click below to see which diseases are transmitted by the Aedes, Culex, and Anopheles mosquitoes.
Mosquito control: can it stop Zika at source?
Source: WHO
Scientists Investigate How Multidrug-Resistant Pathogens are Brought into Hospitals
But where do these pathogens come from? In largest study of its kind in Europe, DZIF scientists from the University of Cologne investigated this question and discovered that almost 10% of patients admitted into hospitals already bring these dreaded pathogens along with them from home.
“We were surprised that on hospital admission almost every tenth patient is colonized with multidrug-resistant pathogens,” explains Dr. Axel Hamprecht from the University of Cologne. He coordinated this study, in which six German university hospitals participated, together with Prof. Harald Seifert, also from the University of Cologne, and colleagues from Charité Berlin. Over 4,000 adults were tested for multidrug-resistant Enterobacteriaceae on admission into hospital by means of stool samples or rectal swabs.
Enterobacteriaceae such as Escherichia coli constitute a normal part of the gut flora and are not pathogenic–as long as they remain in the gut. However, they can cause infections in other organs, for example urinary tract infections. An infection caused by multidrug-resistant bacteria is much more difficult to treat and requires the use of last-resort antibiotics. In their investigations, the researchers paid particular attention to a group of multidrug-resistant bacteria that are often problematic in hospitals: so-called third-generation cephalosporin-resistant Enterobacteriaceae (3GCREB).
These multidrug-resistant gut bacteria which are resistant to cephalosporins, amongst other drugs, have spread worldwide over the past years. Similar to penicillin, cephalosporins are antibiotics that kill bacteria by inhibiting bacterial cell wall synthesis. Newer third-generation cephalosporins are effective against a broad spectrum of bacteria and belong to the group of most commonly used antibiotics. However, over the course of time, the bacteria have defend-ed themselves and have acquired so-called beta-lactamase, an enzyme that renders these antibiotics ineffective. Enterobacteriaceae are transmitted by smear infection, predominantly via faeces and food.
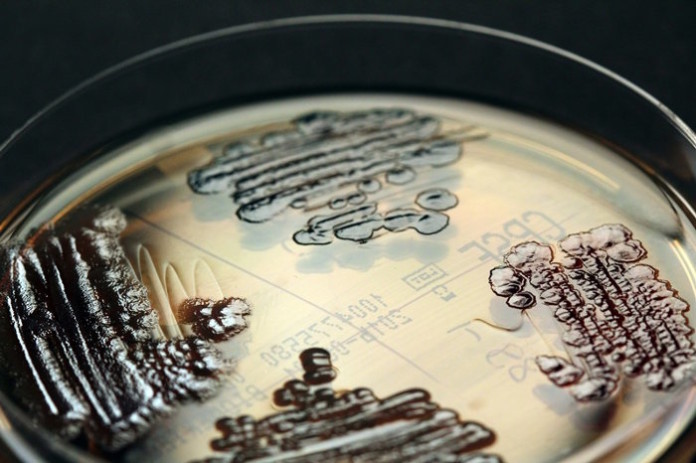
Every tenth patient brings the pathogens into hospital
Out of the 4,376 adults who were tested for 3GCREB pathogens on admission to one of the participating hospitals, 416 were carriers of these multidrug-resistant pathogens. This prevalence is higher than has previously been reported in Germany. Especially often, the scientists found beta-lactamase producing Escherichia coli bacteria, so-called ESBL-producing Entero-bacteriaceae. The prevalence of these multidrug-resistant pathogens differed from hospital to hospital.
In order to elucidate the factors for colonisation with these bacteria, the patients completed a questionnaire on previous hospital stays and lifestyle habits. “Patients who have taken antibiotics and travellers outside Europe are at higher risk,” says Hamprecht, underlining two important research findings.
Experts recommend more hygiene and using fewer antibiotics
What can be done to prevent the spread of multidrug-resistant pathogens as early as possible? Hamprecht is certain, “With so many people affected, the strategy of isolating patients within the hospitals no longer works. Additionally, in contrast to other groups of multidrug-resistant bacteria such as MRSA (Methicillin-resistant Staphylococcus-aureus) strains, standardised sanitation measures for 3GCREB have not been established.” Instead, Hamprecht and Seifert recommend improving hygiene measures in hospitals and practices, a rational use of antibiotics and especially reducing their non-justified administration, as well as more training for doctors.
Source: SciCasts
Invitation to ePoster exhibition
ePoster is an easy way to build an impressive and informative poster without printing costs and shipping efforts.
International Congress on Quality in Laboratory Medicine, 9th – 10th February, 2017. Helsinki, Finland
All congress participants are welcome to present their research results and new, unpublished data as an ePoster in English language. Themes for the posters are requested to relate to the congress themes. Two best ePosters are selected by the Scientific Committee and the awards are given at the Quality Promotion Awards event.
Accepted poster abstracts are also listed in the congress mobile app.
Lab Tests Online Honored With 2016 Digital Health Award
AACC’s public resource on lab testing, Lab Tests Online, has been honored with a 2016 Digital Health Award, which recognizes the world’s best digital health resources. Lab Tests Online was a merit winner in the website category of web-based digital health for consumers produced by associations/professional societies or non-profits. Lab Tests Online was acknowledged from among nearly 500 entrants.
The honor adds to Lab Tests Online’s accolades, and represents its fifteenth award in as many years. Previously, Lab Tests Online has been recognized for excellence in health communications, for its website, and its writing.
The Digital Health Awards is organized by the Health Information Resource Center, a national clearinghouse for professionals who work in consumer health fields. Each year, hundreds of local, state, and national health-related organizations and companies enter the competition.
A panel of health technology professionals reviewed entries based on content, format, success in reaching the targeted health audience, and overall quality, rating each entry on a scale of 1 to 100 points.
Established in 2001, Lab Tests Online is a health information web resource designed to help patients, caregivers, and medical professionals understand the many lab tests that are a vital part of medical care. Laboratory professionals, who are experts in the field, develop and review all content, including articles on lab tests, conditions/diseases, screening, clinical laboratory topics, and lab test news.
Lab Tests Online is available in 14 languages through 17 country sites. The content on each site is translated and adapted to policy and practice specific to that country. Countries with Lab Tests Online sites include the United States/Canada, Australasia, Brazil, China, Czech Republic, France, Germany, Greece, Hungary, Italy, Korea, Poland, Portugal, Romania, Spain, Turkey, and the United Kingdom.
Source: AACC
Magnetic Bacteria Ferry Chemo Drugs to Resistant Tumors
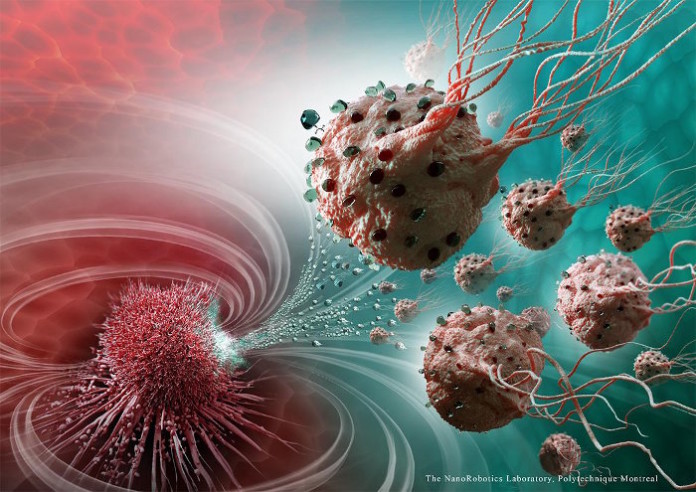
“These legions of nanorobotic agents were actually composed of more than 100 million flagellated bacteria – and therefore self-propelled – and loaded with drugs that moved by taking the most direct path between the drug’s injection point and the area of the body to cure,” said Sylvain Martel, Director of the Polytechnique Montréal Nanorobotics Laboratory, and senior study author.
The technology sounds like science fiction come-to-life. The microbes behind this so-called legions of nanorobots are magnetotactic bacteria (Magnetococcus marinus strain MC-1). Discovered by Richard P. Blakemore in 1975, magnetotactic bacteria are tiny microorganisms that have the capacity to convert iron into magenetite inside organelles called magnetosomes. Each of the magnetite crystal acts as a nano-magnet, and a chain of these act as a built-in compass for north and south detection. The bacteria use these internal compasses to move and align themselves in watery regions with optimal oxygen concentrations.
Martel and his team exploited the unique characteristics of the magnetotactic bacteria to ferry drug-loaded lipososomes into tumors. In particular, M. marinus has a penchant for regions of low oxygen concentration. This makes them ideal carriers of chemotherapy drugs to tumors, since many contain hypoxic regions that are often resistant to therapies.
In mice experiments, Martel and his team showed the nanorobots could deliver drugs in a targeted fashion to colorectal tumors. “The drug’s propelling force was enough to travel efficiently and enter deep inside the tumors,” he added.
The concept of using the bacteria-propelled nanorobots to control and target drug release could potentially minimize the chemotherapy-related collateral damages to the healthy cells. Furthermore, because of higher precision to the tumor, doctors may be able to use a lower dose of the drug to achieve the same potency. This would also curtail side-effects of chemotherapy.
“This innovative use of nanotransporters will have an impact not only on creating more advanced engineering concepts and original intervention methods, but it also throws the door wide open to the synthesis of new vehicles for therapeutic, imaging and diagnostic agents,” said Martel. “Chemotherapy, which is so toxic for the entire human body, could make use of these natural nanorobots to move drugs directly to the targeted area, eliminating the harmful side effects while also boosting its therapeutic effectiveness.”
Source: LabRoots