First review of all available evidence including 172 observational studies looking at how physical distancing, face masks, and eye protection affect the spread of COVID-19, SARS, and MERS in both community and healthcare settings across 16 countries.
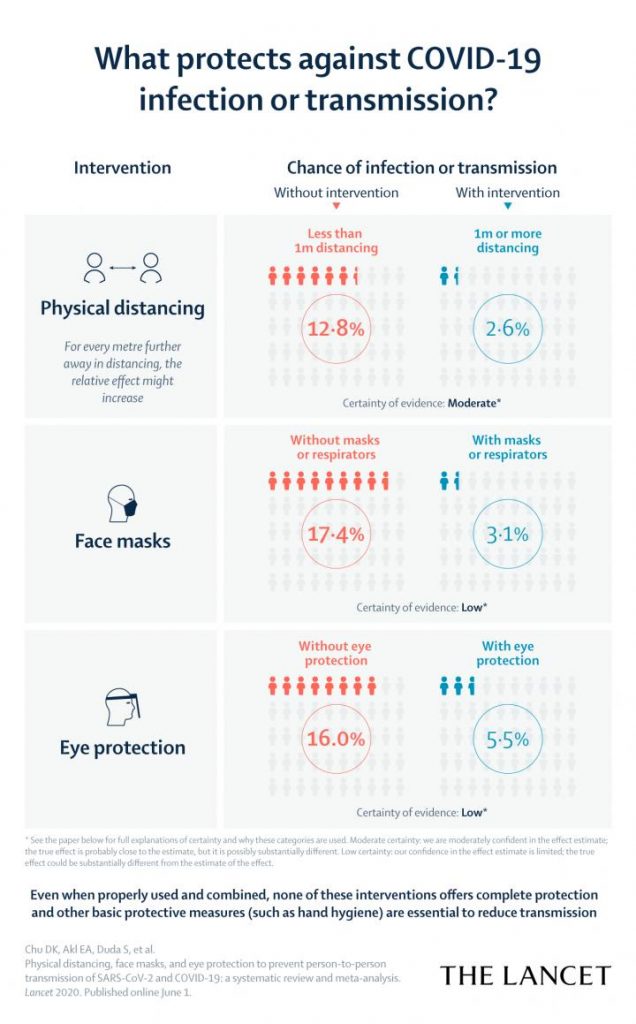
Physical distancing of at least 1 metre lowers risk of COVID-19 transmission, but distances of 2 metres could be more effective.
Face coverings and masks might protect both healthcare workers and the general public against infection with COVID-19, and protective eye covering may also provide additional benefit–although the certainty of the evidence is low for both forms of protection.
Importantly, even when properly used and combined, none of these interventions offers complete protection and other basic protective measures (such as hand hygiene) are essential to reduce transmission.
Keeping at least one metre from other people as well as wearing face coverings and eye protection, in and outside of health-care settings, could be the best way to reduce the chance of viral infection or transmission of COVID-19, according to a systematic review and meta-analysis synthesising all the available evidence from the scientific literature, published in The Lancet.
However, none of these interventions, even when properly used and combined, give complete protection from infection, and the authors note that some of the findings, particularly around face masks and eye protection, are supported by low-certainty evidence [1], with no completed randomised trials addressing COVID-19 for these interventions.
The study, conducted to inform WHO guidance documents, is the first time researchers have systematically examined the optimum use of these protective measures in both community and healthcare settings for COVID-19. The authors say it has immediate and important implications for curtailing the current COVID-19 pandemic and future waves by informing disease models, and standardising the definition of who has been ‘potentially exposed’ (ie, within 2 metres) for contact tracing.
Many countries and regions have issued conflicting advice about physical distancing to reduce transmission of COVID-19, based on limited information. In addition, the questions of whether masks and eye coverings might reduce transmission of COVID-19 in the general population, and what the optimum use of masks in healthcare settings is, have been debated during the pandemic.
“Our findings are the first to synthesise all direct information on COVID-19, SARS, and MERS, and provide the currently best available evidence on the optimum use of these common and simple interventions to help “flatten the curve” and inform pandemic response efforts in the community”, says Professor Holger Schünemann from McMaster University in Canada, who co-led the research. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk.”
The currently best available evidence suggests that COVID-19 is most commonly spread by respiratory droplets, especially when people cough and sneeze, entering through the eyes, nose, and mouth, either directly or by touching a contaminated surface. At the moment, although there is consensus that SARS-CoV-2 mainly spreads through large droplets and contact, debate continues about the role of aerosol spreading.
For the current analysis, an international team of researchers did a systematic review of 172 observational studies assessing distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, SARS, or MERS infection and individuals close to them (eg, caregivers, family, healthcare workers), up to May 3, 2020.
Pooled estimates from 44 comparative studies involving 25,697 participants were included in the meta-analysis. Of these, 7 studies focused on COVID-19 (6,674 participants), 26 on SARS (15,928), and 11 on MERS (3,095).
The COVID-19 studies included in the analysis consistently reported a benefit for the three interventions and had similar findings to studies of SARS and MERS.
Analysis of data from nine studies (across SARS, MERS and COVID-19, including 7,782 participants) looking at physical distance and virus transmission found that keeping a distance of over one metre from other people was associated with a much lower risk of infection compared with less than one metre (risk of infection when individuals stand more than a metre away from the infected individual was 3% vs 13% if within a metre), however, the modelling suggests for every extra metre further away up to three metres, the risk of infection or transmission may halve (figure 3). The authors note that the certainty of their evidence on physical distancing is moderate [1] and that none of the studies quantitatively evaluated whether distances of more than 2 metres were more effective, although meta-analyses provided estimates of risk.
Thirteen studies (across all three viruses, including 3,713 participants) focusing on eye protection found that face shields, goggles, and glasses were associated with lower risk of infection, compared with no eye covering (risk of infection or transmission when wearing eye protection was 6% vs 16% when not wearing eye protection). The authors note that the certainty of the evidence for eye coverings is low [1].
Evidence from 10 studies (across all three viruses, including 2,647 participants) also found similar benefits for face masks in general (risk of infection or transmission when wearing a mask was 3% vs 17% when not wearing a mask). Evidence in the study was looking mainly at mask use within households and among contacts of cases, and was also based on evidence of low certainty [1].
For healthcare workers, N95 and other respirator-type masks might be associated with a greater protection from viral transmission than surgical masks or similar (eg, reusable 12-16 layer cotton or gauze masks). For the general public, face masks are also probably associated with protection, even in non-health-care settings, with either disposable surgical masks or reusable 12-16 layer cotton ones. However, the authors note that there are concerns that mass face mask use risks diverting supplies from health-care workers and other caregivers at highest risk for infection.
They also stress that policy makers will need to quickly address access issues for face masks to ensure that they are equally available for all. “With respirators such as N95s, surgical masks, and eye protection in short supply, and desperately needed by healthcare workers on the front lines of treating COVID-19 patients, increasing and repurposing of manufacturing capacity is urgently needed to overcome global shortages”, says co-author Dr Derek Chu, Assistant Professor at McMaster University. “We also believe that solutions should be found for making face masks available to the general public. However, people must be clear that wearing a mask is not an alternative to physical distancing, eye protection or basic measures such as hand hygiene, but might add an extra layer of protection.”
The authors also stress the importance of using information about how acceptable, feasible, resource intense, and equally accessible to all the use of these interventions are when devising recommendations. “Across 24 studies of all three viruses including 50,566 individuals, most participants found these personal protection strategies acceptable, feasible, and reassuring, but noted harms and challenges including frequent discomfort and facial skin breakdown, increased difficulty communicating clearly, and perceived reduced empathy from care providers by those they were caring for”, says Dr Sally Yaacoub from the American University of Beruit in Lebanon.
According to co-author Karla Solo from McMaster University in Canada: “While our results provide moderate and low certainty evidence, this is the first study to synthesise all direct information from COVID-19 and, therefore, provides the currently best available evidence to inform optimum use of these common and simple interventions.”
Despite these important findings, the review has some limitations including that few studies assessed the effect of interventions in non-healthcare settings, and most evidence came from studies of SARS and MERS. Finally, the effect of duration of exposure on risk for transmission was not specifically examined.
Writing in a linked Comment, lead author Professor Raina MacIntyre (who was not involved in the study) from the Kirby Institute, University of New South Wales in Australia, describes the study as “an important milestone”, and writes, “For health¬care workers on COVID¬19 wards, a respirator should be the minimum standard of care. This study by Chu and colleagues should prompt a review of all guidelines that recommend a medical mask for health workers caring for COVID¬19 patients. Although medical masks do protect, the occupational health and safety of health workers should be the highest priority and the precautionary principle applied.”
She continues, “[They] also report that respirators and multilayer masks are more protective than are single layer masks. This finding is vital to inform the proliferation of home¬made cloth mask designs, many of which are single¬layered. A well designed cloth mask should have water¬resistant fabric, multiple layers, and good facial fit…Universal face mask use might enable safe lifting of restrictions in communities seeking to resume normal activities and could protect people in crowded public settings and within households.”
NOTES TO EDITORS
The study was in part funded by the World Health Organization. It was conducted by researchers at McMaster University, Canada; the American University of Beirut, Lebanon; German Hospital of Buenos Aires, Argentina; Southlake Regional Health Centre, Canada; University of British Columbia, Canada; McMaster University, Canada; The Research Institute of St. Joe’s Hamilton, Canada; Pontificia Universidad Católica de Chile, Chile; Beijing University of Chinese Medicine, China; Dongzhimen Hospital, China; Guangzhou University of Chinese Medicine, The Fourth Clinical Medical College, China; China academy of Chinese Medical Science, China; American University of Beirut, Lebanon; Rafik Hariri University Hospital, Lebanon; The London School of Hygiene & Tropical Medicine, UK; University of Hull, UK.
[1] This study used GRADE categories of evidence. These include: high certainty (ie, we are very confident that the true effect lies close to that of the estimate of the effect); moderate certainty (we are moderately confident in the effect estimate; the true effect is probably close to the estimate, but it is possibly substantially different); low certainty (our confidence in the effect estimate is limited; the true effect could be substantially different from the estimate of the effect); very low certainty (we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect).
Source: The Lancet









