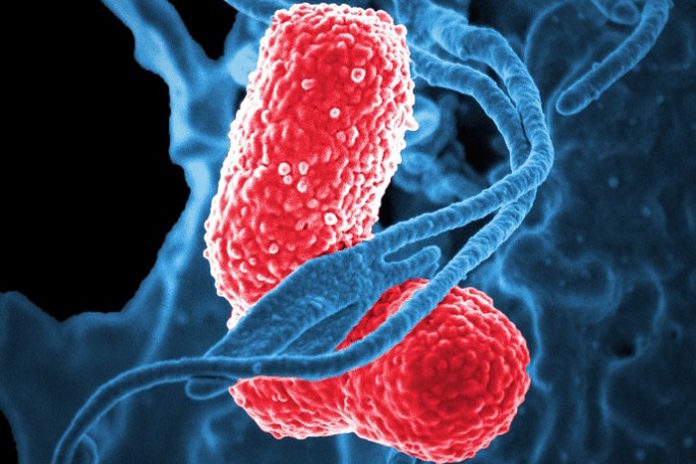
The bacterium, estimated to be the third most common cause of hospital-acquired infections in the United States in a recent study, can cause a wide range of infections such as pneumonia, bacteremia, wound or surgical site infections and urinary tract infections. What’s more, Klebsiella pneumoniae is rapidly becoming resistant to all known antibiotics; resistant forms are considered an urgent threat to public health by the Centers for Disease Control and Prevention.
What scientists have known about the organism is that it secretes small molecules called siderophores that enable it to acquire iron from a host and fuel its spread. Siderophores are thought to worsen infection by promoting bacterial growth. But a new study in mBio this week demonstrates that siderophores do even more to help Klebsiella invade.
In mice infected with K. pneumoniae, siderophores caused the animals to turn on proteins that increase inflammation and activated a master protein called HIF-1 alpha that paved the way for bacteria to spread from the lungs to the spleen. HIF-1 alpha controls the ability of substances to pass through blood vessels and inflammatory gene expression.
“We’ve known for a long time that siderophores are critical for bacteria to cause infection, because they steal iron from the host to grow,” says senior study author Michael Bachman, M.D., Ph.D., assistant professor of clinical pathology and associate director of the Clinical Microbiology Laboratory at the University of Michigan in Ann Arbor. “This study sheds some light on the consequences of that. When the bacterium steals this iron, what’s likely happening is the host cells are becoming stressed and are inducing inflammation and cell signaling pathways that actually worsen the infection by allowing the bacteria to escape from the lungs to the spleen.”
A barrier to studying siderophores in vivo in the past, Bachman says, is that they allow bacterial proliferation, which in turn may increase inflammation, tissue damage and bacterial dissemination. “What we tried to do was control for levels of bacteria, and then compare infections in which the Klebsiella made siderophores and in which it didn’t,” he explains. To study the effects of siderophore secretion independent of increased bacterial growth, Bachman’s team employed tonB mutants capable of disrupting normal use of siderophores, so the organism could secrete siderophores but not use them.
The investigators infected mice with either a strain of K. pneumoniae that makes three siderophores called enterobactin (Ent), salmochelin (Sal) and yersiniabactin (Ybt), or a mutant form of the bacterium that could not produce siderophores. Mice infected with the siderophore-producing strain had more bacteria invading from the lung to the spleen and they activated the cytokines IL-6, CXCL1 and CXCL2.
“We had assumed that siderophores simply helped the bacteria grow more, triggering more inflammation and spread,” Bachman says. “Now we know siderophores can trigger these effects directly.”
Additional laboratory experiments in the mice revealed that all three siderophores were required for the most bacterial dissemination to the spleen; that siderophores secreted by K. pneumoniae stabilized HIF-1 alpha; and that the presence of HIF-1 alpha in endothelial cells in the lungs is required for the bacteria to spread to the spleen. Mice that produced HIF-1 alpha and were infected with K. pneumoniae had more bacterial invasion to the spleen than mice that did not produce HIF-1 alpha and were similarly infected.
“These results indicate that bacterial siderophores directly alter the host response to pneumonia in addition to providing iron for bacterial growth,” Bachman said. “Therapies that disrupt production of siderophores could provide a two-pronged attack against K. pneumoniae infection by preventing bacterial growth and preventing bacterial dissemination to the blood.”
Source: ASM